-
 Agriculture & Food
Agriculture & Food
-
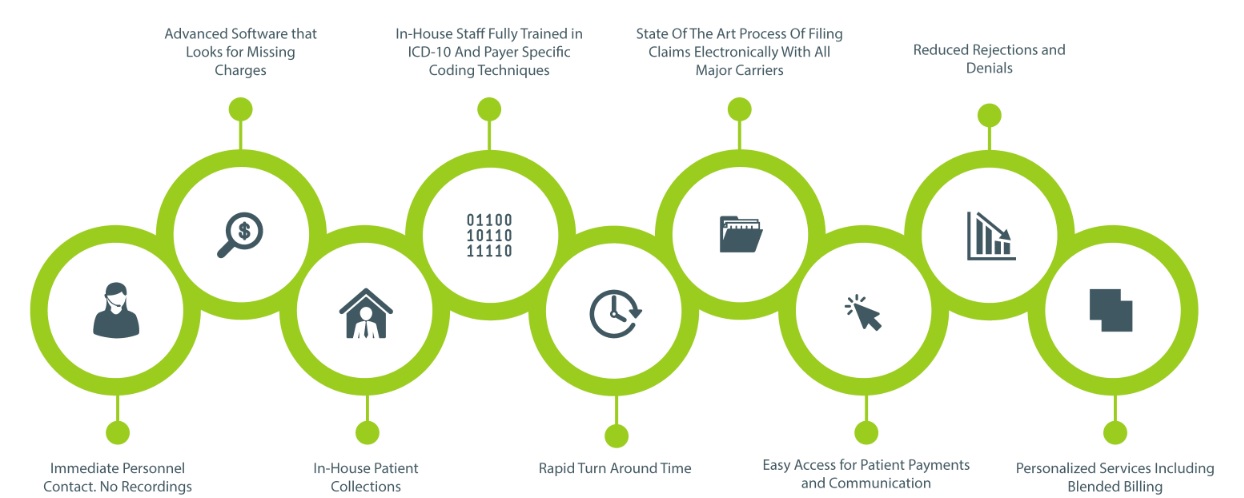
 Business Services
Business Services
- Accounting
- Advertising
- Aerospace and Defense
- Agriculture and Forestry
- Arts and Entertainment
- Associations
- Auctioneers
- Automotive
- Banking services
- Biotechnology and Pharmaceuticals
- Brokers
- Business and Society
- Business centres
- Business Services
- Cleaning equipment & Services
- Conferences and Events
- Construction and Maintenance
- Consultants
- Consumer Goods and Services
- Cooperatives
-
 Electronics, IT and Telecoms
Electronics, IT and Telecoms
-
 Leisure & Tourism
Leisure & Tourism
-
 Minerals
Minerals
- Analytical Techniques & Applied Mineralogy
- Biotechnology
- Comminution
- Control & Instrumentation
- Electrometallurgy
- Environmental Issues
- Froth Flotation
- General Minerals Engineering
- Gravity Concentration
- Hydrometallurgy
- Magnetic/Electrical Separation
- Materials Handling
- Metal Detector
- mineral
- Pyrometallurgy
- Reagents
- Sizing & Classification
- Solid-Liquid Separation
-
 Textiles, Clothing, Leather,
Textiles, Clothing, Leather,
-
 Transport & Logistics
Transport & Logistics
More
-
Africa
-
Central Africa
-
Cameroon
(1201) -
Angola
(616) -
Gabon
(186) -
Sao Tome and Principe
(86) -
Equatorial Guinea
(54) -
Congo, Democratic Republic of the
(38) -
Central African Republic
(22) -
Chad
(17) -
Congo, Republic of the
(10)
-
-
Eastern Africa
-
Kenya
(5061) -
Zimbabwe
(1970) -
Mauritius
(1029) -
Uganda
(1007) -
Ethiopia
(450) -
Zambia
(384) -
Mozambique
(317) -
Madagascar
(304) -
Rwanda
(290) -
Seychelles
(172) -
Malawi
(166) -
Somalia
(160) -
Tanzania, United Republic of
(87) -
Burundi
(54) -
Djibouti
(46) -
Comoros
(7) -
Eritrea
(4)
-
-
Northern Africa
-
Egypt
(8859) -
Morocco
(4215) -
Tunisia
(2327) -
Algeria
(1643) -
Sudan
(354) -
Libyan Arab
(89) -
South Sudan
(35)
-
-
Southern Africa
-
South Africa
(9389) -
Namibia
(292) -
Botswana
(242) -
Swaziland
(59) -
Lesotho
(22)
-
-
Western Africa
-
Nigeria
(7160) -
Ghana
(1934) -
Senegal
(734) -
Benin
(320) -
Togo
(167) -
Burkina Faso
(136) -
Mali
(116) -
Guinea
(97) -
Cape Verde
(86) -
Cote d
(84) -
Sierra Leone
(81) -
Liberia
(64) -
Mauritania
(44) -
Niger
(41) -
Gambia, The
(34) -
Guinea-Bissau
(16)
-
-
-
Americas
-
Central America
-
Mexico
(24649) -
Costa Rica
(2786) -
Panama
(1980) -
Guatemala
(1300) -
El Salvador
(635) -
Honduras
(612) -
Nicaragua
(456) -
Belize
(369)
-
-
North America
-
United States
(2553205) -
Canada
(197781) -
Trinidad and Tobago
(519) -
Saint Vincent and the Grenadines
(334) -
Saint Lucia
(239) -
Turks and Caicos Islands
(113) -
Bahamas, The
(50) -
Saint Kitts and Nevis
(31)
-
-
South America
-
The Caribbean
-
Dominican Republic
(1465) -
Jamaica
(751) -
Cuba
(216) -
Barbados
(215) -
Haiti
(87) -
Antigua and Barbuda
(78) -
Montserrat
(50) -
Dominica
(36) -
Grenada
(26) -
Saint Barthelemy
(3)
-
-
-
Asia
-
Central Asia
-
Singapore
(15175) -
Uzbekistan
(534) -
Bhutan
(77)
-
-
East Asia
-
Northern Asia
-
South Asia
-
Sri Lanka
(3281)
-
-
South East Asia
-
Myanmar
(842)
-
-
Middle East
-
United Arab Emirates
(25768) -
Iran
(9791) -
Israel
(7348) -
Saudi Arabia
(6508) -
Lebanon
(2947) -
Jordan
(2706) -
Qatar
(2241) -
Kuwait
(1849) -
Oman
(1321) -
Bahrain
(1285) -
Iraq
(780) -
Yemen
(171) -
Palestine, State of
(53) -
Syrian Arab Republic
(45)
-
-
-
Europe
-
Central Europe
-
Eastern Europe
-
Northern Europe
-
South East Europe
-
Bosnia and Herzegovina
(1149)
-
-
South West Europe
-
Southern Europe
-
Western Europe
-
United Kingdom
(315494) -
Germany
(161441) -
Netherlands
(147075) -
Spain
(140726) -
France
(123052) -
Italy
(119920) -
Belgium
(49875) -
Denmark
(34510) -
Poland
(24916) -
Ireland
(22942) -
Portugal
(21531) -
Finland
(20008) -
Romania
(16092) -
Greece
(14117) -
Hungary
(13481) -
Czech Republic
(9005) -
Bulgaria
(6922) -
Slovakia
(6164) -
Estonia
(5123) -
Slovenia
(4449) -
Cyprus
(2613) -
Malta
(1478)
-
-
-
Oceania
-
Australasia
-
Australia
(48125) -
New Zealand
(8771)
-
-
Melanesia
-
Fiji
(974) -
Papua New Guinea
(237) -
New Caledonia
(213) -
Vanuatu
(59) -
Solomon Islands
(17)
-
-
Micronesia
-
Palau
(1169) -
Micronesia, Federated States of
(276) -
Kiribati
(54) -
Marshall Islands
(16) -
Nauru
(6)
-
-
Polynesia
-